Dental implant is a popular and an effective tooth restoration technique. Made using titanium, dental implants are placed carefully in the jawbone and integrated with the natural bone to provide a sturdy foundation for tooth replacement. It is the most sought-after treatment for tooth restoration in clinical dentistry primarily because of it mechanical and biological properties.
Good oral hygiene is equally important after getting dental implants as the prevalence rate of inflammation around the dental implant is relatively high. The condition is better known as the Peri-Implant disease.
Understanding the Peri-Implant Disease
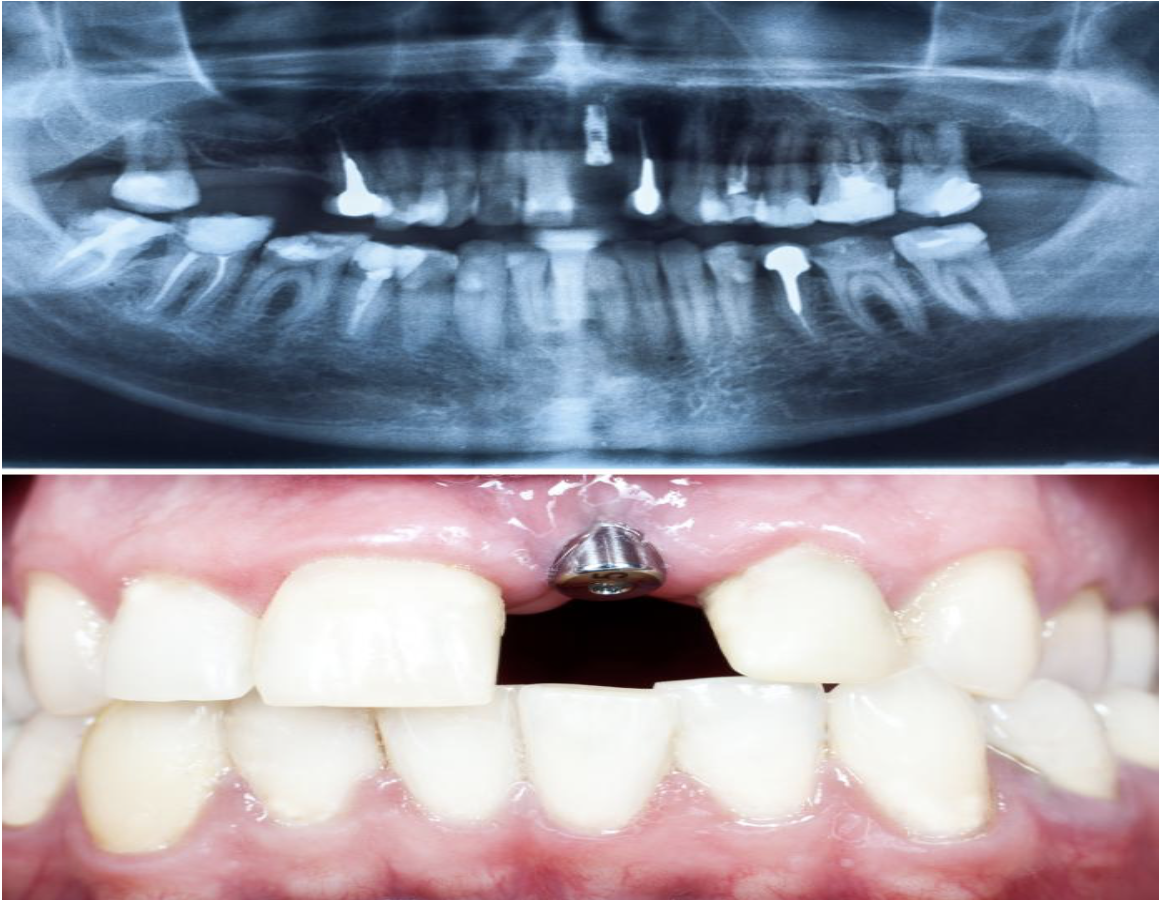
Peri-implant disease can be best described as an inflammatory condition. This condition affects both hard and soft gum tissues near dental implants. This is caused due to poor oral hygiene and implant maintenance. The bacteria begin to build-up on the implant’s base, right below the gum line. The bacterial growth irritates the gum tissue overtime. This causes inflammation in the gums and damages the tissue. If the problem is not addressed immediately, it can lead to bone loss and eventually dental implant loss. Though it resembles periodontal infection, the treatment options for peri-implant disease are different.
Types of Peri-Implant Disease
The peri-implant disease is of two types—peri-implant mucositis and peri-implantitis. Let’s take a closer look at the two types of peri-implant disease to develop a better understanding:
- Peri-Implant Mucositis
The peri-implant mucositis basically manifests in the soft tissue. The signs are similar to gingivitis. It causes swelling, redness and inflammation but is only confined to soft tissues. It can be best treated if it is detected early by calculus and biofilm removal. In other words, treatment of peri-implant mucositis is non-invasive and simpler as compared to peri-implantitis. So, far there is no evidence of bone loss due to peri-implant mucositis; however, it is a precursor of peri-implantitis.
- Peri-Implantitis
In this type of peri-implant disease, gum inflammation occurs around the soft tissue that leads to deterioration of the bone that supports the dental implant. It is also described as a serious and destructive inflammatory dental process in clinical dentistry. It promotes both peri-implant hard and soft tissue loss affecting osseo-integration.
Diagnostic considerations that have been proposed for the timely detection of peri-implantitis disease include probing, suppuration, pre or post radiographs, microbiological testing and mobility. Initial dental implant probing must be performed once the restoration is properly installed with the help of the conventional periodontal probe with light force. Mobility and radiographs can also be used to supplement its diagnosis.
Peri-implantitis is sometimes compared to periodontal disease because of its inflammatory nature. However, one of the most important differences between the two is that peri-implantitis has the tendency to develop on the lingual and facial aspects of the dental implant in such a way that it is undetectable and hard to identify using traditional radiographs. Studies show that in this case, the most effective technology is the cone beam computed tomography. It is proven for identifying lingual, proximal bony and lingual lesions surrounding dental implants. The diagnosis for peri-implantitis is aided by acquiring baseline bone level 360-degree scans of the implants. If peri-implantitis condition is suspected, CBCT scans are compared with baseline scans to determine the definitive bone loss including the severity and location.
Though the presence of pathogenic biofilm is the top factor, local and systemic factors should also be identified as all these factors can lead to the development as well as progression of peri-implant disease. Systemic factors include smoking, diabetes and immunosuppression while local factors include excessive occlusal forces or residual cement.
In most cases, surgical therapy is advised to patients with moderate & severe peri-implantitis. It provides access for proper cleaning and also helps develop an environment that enable patients to both maintain and reconstruct lost tissue.
Statistics show that 80 percent of the people with dental implants develop peri-implant mucositis and that nearly 56 percent suffer from peri-implantitis.
For more information about peri-implant disease or if you are experiencing inflammation around implants, get in touch with us today. Call (208) 342-0315 to schedule an appointment with our experienced periodontist for a proper oral examination and diagnosis.